Medically Reviewed by: Dr. Sonali Pandey– DCH, MBBS, DNB Paediatrics
Neonatal nutrition is a critical aspect of care, particularly for premature babies who enter the world before they are fully developed. The journey of a premature baby is marked by unique challenges and considerations, and one of the most fundamental aspects of their care is ensuring they receive the Neonatal Nutrition necessary for optimal growth and development. In this blog, we will delve into the key considerations surrounding neonatal nutrition for premature babies, exploring the importance of proper nourishment, the challenges they face, and the specialized strategies and techniques employed to support their nutritional needs.
Understanding the intricacies of neonatal nutrition is essential for healthcare professionals and parents alike, as it plays a vital role in setting the foundation for the health and well-being of these fragile infants. Let us embark on a journey to explore the world of neonatal nutrition and its significance in the care of premature babies.
Also Read: Managing Common Infections in Newborns
Understanding Premature Babies
Premature birth, also referred to as preterm birth, happens when a baby is born before completing 37 weeks of pregnancy. There are three sub-categories based on gestational age:
- Extremely preterm: Less than 28 weeks
- Very preterm: 28 to less than 32 weeks
- Moderate to late preterm: 32 to 37 weeks
Premature babies typically exhibit the following characteristics:
- Small size, often with a disproportionately large head
- Thin, translucent skin due to a lack of body fat
- Immature respiratory and digestive systems
- Risk for long-term health and developmental issues, including learning disabilities, vision, and hearing impairments, as well as behavioral and mental health challenges.
Various Maternal factors contribute to premature birth, such as:
- Infections
- Chronic conditions like high blood pressure and diabetes
- Lifestyle factors such as smoking and substance abuse
- Multiple pregnancies
- Physical injury or trauma.
Preterm babies spend the initial days in the NICU because of special requirements like respiratory support & other systemic needs. The earlier the birth, the higher the risks of health challenges.
Premature babies have distinct nutritional needs because of their underdeveloped organ systems and increased nutritional requirements for growth and development. They may require specialized feeding methods and fortified breast milk or formula to fulfill these needs. In some cases, intravenous (IV) nutritional support may be necessary to ensure adequate nutrient intake.
Parents and caregivers of premature babies must collaborate closely with healthcare providers to address their specific nutritional requirements and ensure they receive appropriate feeding and nutritional assistance.
Nutritional Challenges for Premature Babies
- Difficulty with sucking, swallowing, and breathing coordination:
- Premature infants often struggle with underdeveloped sucking and swallowing reflexes, leading to feeding difficulties and an increased risk of aspiration.
- Alternative feeding methods like gavage feedings may be necessary to ensure adequate nutrition while minimizing respiratory complications.
- Immature digestive systems and gastrointestinal issues:
- Premature babies have immature digestive systems, making it challenging for them to tolerate and digest full feedings.
- Feeding intolerance can result, potentially causing suboptimal nutrient intake and slower growth.
- There’s a heightened risk of gastrointestinal complications such as necrotizing enterocolitis (NEC), particularly among preterm infants.
- Increased nutrient needs for growth and development:
- Premature babies require higher nutrient levels to support their rapid growth and development, given their depleted nutrient reserves from a shorter time in the womb.
- Fulfilling these increased nutrient requirements is crucial to prevent growth failure and promote positive long-term developmental outcomes.
- Human milk, especially from the baby’s mother, is preferred due to its tailored nutrients and various health benefits, including reduced rates of NEC and improved neurodevelopmental outcomes.
- Comprehensive and individualized approach:
- Addressing these nutritional challenges requires a personalized approach, involving specialized feeding techniques, nutritional supplements, and close monitoring of growth and development.
- Healthcare providers play a vital role in supporting premature infants’ nutritional needs and guiding parents through the complexities of neonatal feeding and nutrition.
Also Read: Neonatal Jaundice: Causes, Symptoms, and Treatment
Feeding Strategies and Techniques
Feeding premature babies in the neonatal intensive care unit (NICU) requires specialized approaches to cater to their unique nutritional needs and foster growth. These strategies encompass:
I. Intravenous Nutrition:
- For extremely premature infants, immediate intravenous nutrition may be vital to supply essential nutrients and aid growth until they can tolerate enteral feeding.
II. Early Enteral Feeding:
- Introducing enteral feeding as soon as the infant’s condition allows, aiming to deliver nutrition via the gastrointestinal tract. This is crucial for encouraging optimal growth and development while minimizing risks like necrotizing enterocolitis (NEC).
III. Complete Nutrition to Support Growth:
- The objective is to mimic intrauterine growth rates by providing preterm infants with enriched diets, fortified milk, or specialized preterm formulas. This ensures they receive vital nutrients to support brain development and overall growth.
Breast Milk vs. Formula
Breast milk offers a multitude of advantages for premature babies, including:
- Nutritional Benefits: Breast milk is uniquely formulated to fulfill the precise nutritional requirements of premature infants, fostering optimal growth and development.
- Immune Protection: It contains antibodies, enzymes, and other components that bolster the immune system of preterm infants, shielding them from infections and lowering the likelihood of conditions like necrotizing enterocolitis (NEC).
- Neurodevelopmental Advantages: Studies indicate that feeding premature babies maternal milk may yield long-term neurodevelopmental perks, such as enhanced IQ, improved academic performance, and reduced ADHD symptoms.
Challenges and considerations for breastfeeding premature babies include:
- Developing Feeding Skills: Premature infants often possess underdeveloped sucking and swallowing reflexes, posing difficulties in breastfeeding effectively.
- Limited Milk Production: Mothers of premature babies may initially produce insufficient milk quantities, necessitating support, and interventions to establish and sustain an ample milk supply.
- Prolonged Hospital Stays: Preterm infants typically undergo extended hospitalization, which may impede breastfeeding initiation and hinder maternal-infant bonding.
When maternal breast milk is unavailable, donor breast milk or formula feeding serves as alternative options. Formula feeding ensures consistent nutrient delivery, yet it carries a heightened risk of NEC compared to donor breast milk feeding. In instances where donor breast milk is inaccessible, formula feeding becomes necessary. In such scenarios, healthcare providers meticulously assess the preterm infant’s nutritional needs and health status to determine the most suitable feeding regimen.
Healthcare providers play a pivotal role in assisting parents in making well-informed decisions regarding feeding choices for their premature babies, considering the potential benefits and risks associated with each approach.
Techniques for Supporting Oral Feeding Development:
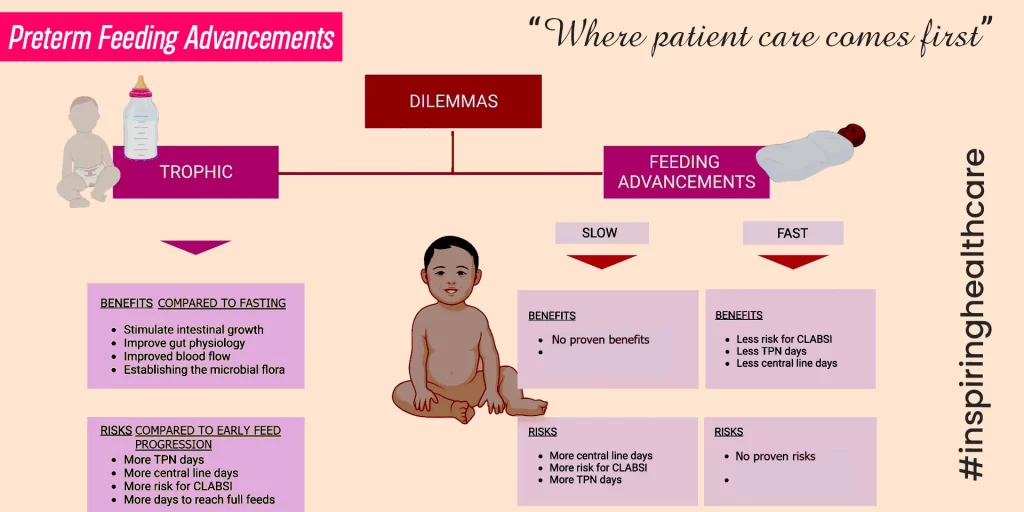
I. Trophic Feeding:
- Administering small amounts of enteral milk with minimal nutritional value to stimulate postnatal gastrointestinal development, often in conjunction with total parenteral nutrition.
II. Pacing and Positioning:
- Employing specific techniques during feeding, such as creating a calm environment, adjusting feeding positions, and allowing babies to feed at their own pace. This prevents fatigue and ensures safe, effective, and enjoyable feeding experiences.
III. Tube Feeding or Palade Feeding:
- In cases where breastfeeding needs augmentation, alternate methods like tube feeding or palate feeding may be necessary to ensure adequate nutrition.
Monitoring Growth and Adjusting Feeding Plans:
I. Regular Growth Assessments:
- Consistently monitor the baby’s weight, length, and head circumference to track growth and detect any signs of growth restriction or inadequate weight gain.
II. Nutritional Support and Supplementation:
- Modifying feeding plans, enriching breast milk, or providing additional nutritional support to address specific growth and development requirements and prevent long-term complications associated with insufficient nutrition.
III. Multidisciplinary Care:
- Involving a team of healthcare professionals, including neonatologists, dietitians, and feeding specialists, to collaboratively assess and manage the baby’s nutritional needs and growth progress.
By implementing these strategies and techniques, healthcare providers can effectively support the optimal nutrition and feeding development of premature babies, fostering healthy growth and long-term well-being.
Potential Long-Term Implications of Early Nutrition
- Impact on Neurodevelopmental Outcomes
- Research indicates that early nutrition significantly influences cognitive function, behavior, and mental health.
- Inadequate nutrition during critical brain development stages may lead to lasting cognitive deficits, learning disabilities, and behavioral problems.
- Conversely, optimal nutrition, particularly through breastfeeding, is associated with improved cognitive function, academic achievement, and reduced risk of attention-deficit/hyperactivity disorder (ADHD).
- Relationship with Metabolic Health
- Early nutrition plays a crucial role in shaping metabolic health, impacting the likelihood of obesity, diabetes, and cardiovascular diseases in later life.
- Undernutrition during pivotal development phases can trigger metabolic adaptations that increase the risk of obesity and related disorders.
- Conversely, excessive intake of energy-dense foods during early life can also elevate the risk of obesity and related metabolic issues.
- The provision of appropriate energy and nutrients during infancy is essential to prevent such negative outcomes and promote long-term metabolic well-being.
- Importance of Ongoing Nutritional Support
- Continuous nutritional support beyond infancy is vital for promoting optimal growth and preventing long-term health complications.
- This includes sustained breastfeeding or appropriate formula feeding, introduction of complementary foods, and ongoing monitoring of growth and nutritional status.
- Healthcare providers play a critical role in supporting the nutritional needs of infants and young children, guiding parents in making informed decisions about feeding practices to ensure long-term health and well-being.
If you are seeking consultation, visit Sanjivini Super Specialty Hospital and book your appointment now!


Pingback: Neonatal Nutrition: Key Considerations for Prem...