Medically Reviewed by: Dr. Sonali Sharma MD- GYNAE & OBS
Gynecological Cancers are a significant health concern for women globally, affecting millions annually. In this blog, we’ll explore the various types of gynecological cancers, their risk factors, symptoms, and available treatments. By understanding these diseases, we aim to empower readers to prioritize their gynecological health and take proactive steps toward prevention and early detection.
Overview of Gynecological Cancers
Gynecological cancers refer to malignant tumors that develop in a woman’s reproductive organs, primarily within her pelvic region. These cancers encompass cervical, ovarian, uterine (endometrial), vaginal, and vulvar cancers.
Common risk factors contribute to an elevated risk across various types of gynecological cancers:
- Age: Risks tend to increase with age.
- Obesity: Linked to higher rates of ovarian cancer.
- Long-term use of hormone replacement therapy: Associated with an increased risk of Breast cancer.
- Smoking
- A positive Family history: Suggestive of inherited genetic syndromes like BRCA1/BRCA2.
Early detection and screening are paramount for improving patient outcomes, particularly for cervical cancer, for which established screening methods like Pap smear and HPV testing exist. While screening options for other gynecological cancers are more limited, recognizing warning signs and discussing personal risk factors and potential interventions with healthcare providers are essential steps. Primary care practitioners play a crucial role in identifying symptoms and referring patients for timely evaluation and management.
Also Read: The Importance of Regular Gynecological Check-ups
Types of Gynecological Cancers
Cervical Cancer
Cervical cancer ranks as the fourth most prevalent cancer among women worldwide, with approximately 604,000 new cases and nearly 342,000 deaths reported in 2020. This disease disproportionately affects women in low-income countries. The primary cause is the infection of high-risk human papillomavirus (HPV).
Risk Factors: Several factors increase the risk of cervical cancer, including early initiation of sexual activity, multiple sexual partners, a history of sexually transmitted infections, an immunocompromised state (such as being HIV positive), low socioeconomic status, and poor nutrition.
HPV Infection: Almost all cervical cancers are linked to high-risk HPV strains, notably HPV16 and HPV18. Alarmingly, around 85% of cervical cancer deaths occur in underdeveloped or developing countries.
Symptoms and Signs: Cervical cancer often manifests initially with minimal symptoms. However, warning signs may include abnormal bleeding during or after sexual intercourse, postmenopausal bleeding, and unusual vaginal discharge.
Screening Methods: The two primary screening methods for cervical cancer are the Pap smear and HPV test. The Pap smear involves examining cells collected from the cervix to detect any abnormalities, while the HPV test identifies the presence of high-risk HPV DNA in cervical samples.
Treatment Options: Treatment for cervical cancer depends on the disease’s stage and severity. Options include surgery, chemotherapy, radiation therapy, targeted therapies, and immunotherapies.
Prevention Strategies: Preventive measures for cervical cancer include HPV vaccination, regular screening to detect precancerous conditions early, practicing safe sex by using condoms, and limiting sexual partners.
Global Initiatives: The World Health Organization aims to eradicate cervical cancer as a public health concern by 2030 through widespread vaccination, screening, and treatment programs.
By understanding the risk factors, symptoms, screening methods, and prevention strategies outlined above, individuals can take proactive steps to protect themselves against cervical cancer and contribute to its global elimination.
Also Read: The Dos and Don’ts of Intimate Hygiene: A Guide for Gen Z Women
Ovarian Cancer
Ovarian Cancer ranks as the seventh most common among women worldwide, bearing a high mortality burden. It is a type of cancer that originates in the ovaries, fallopian tubes, or peritoneum. It involves the growth of cells that multiply quickly and can invade healthy tissues.
- Risk Factors: Various factors contribute to the risk of ovarian cancer, including family history, age, and reproductive history (such as nulliparity or infertility). Genetic predispositions also play a significant role, with rare inherited mutations amplifying susceptibility.
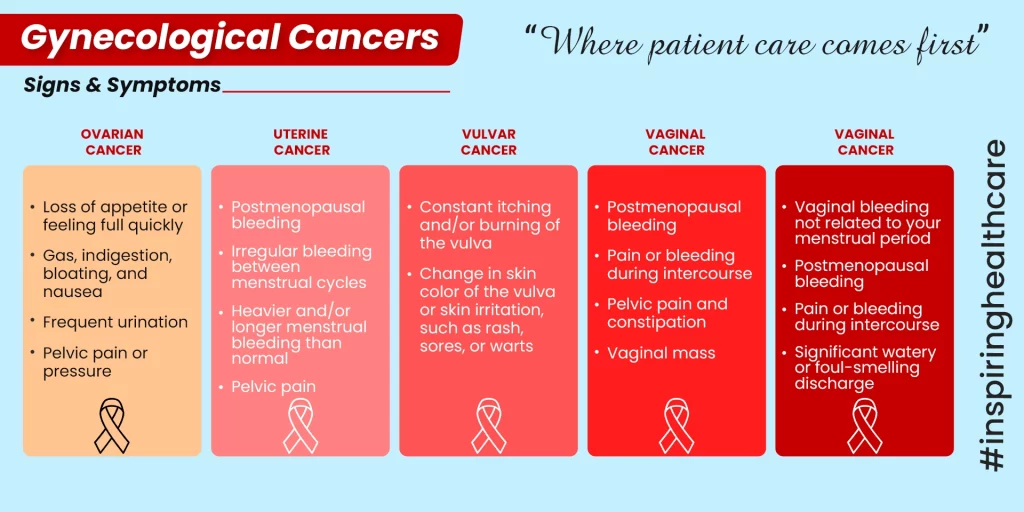
- Symptoms and Signs: Symptoms of ovarian cancer can be vague but may encompass bloating, pelvic discomfort, alterations in bowel habits, and unusual fatigue. Notably, early-stage ovarian cancer often manifests with mild or no symptoms, posing challenges for timely detection.
- Challenges in Early Detection: The early detection of ovarian cancer remains arduous due to the absence of specific symptoms during the initial stages. Consequently, diagnoses frequently occur at advanced stages, when treatment options are constrained. Screening methodologies like CA-125 blood tests and ultrasounds have inherent limitations in identifying early-stage disease.
- Treatment Options: The treatment approach for ovarian cancer typically integrates surgery, chemotherapy, and occasionally targeted therapies, tailored to the disease stage and extent. Surgery aims to excise as much tumor tissue as feasible, while chemotherapy endeavors to eradicate any remaining cancer cells. Targeted therapies concentrate on specific molecular vulnerabilities within cancer cells, enhancing treatment precision.
Uterine (Endometrial) Cancer
Endometrial cancer ranks as the most prevalent gynecologic cancer in the United States, comprising 7% of all cancer cases. It is estimated that in 2024, approximately 67,880 new cases of uterine corpus cancer, inclusive of endometrial cancer, will be diagnosed in the country.
Risk factors for endometrial cancer encompass estrogen exposure, obesity, and advancing age. Additionally, factors like family medical history and reproductive background contribute to its development.
Indications of endometrial cancer may manifest as abnormal vaginal bleeding and pelvic discomfort. Timely detection significantly enhances prognosis.
Diagnostic approaches for endometrial cancer include endometrial biopsy and imaging techniques such as CT scans or MRIs, pivotal in gauging disease extent.
Treatment modalities hinge on cancer stage and attributes. Common interventions comprise:
- Surgery: Typically entails hysterectomy alongside fallopian tube and ovary removal.
- Radiation Therapy: Postoperative application reduces recurrence risk.
- Chemotherapy: Recommended for advanced or recurrent instances.
A comprehensive understanding of risk factors, symptoms, diagnostics, and treatment options is imperative for effective endometrial cancer management, leading to enhanced patient outcomes.
Also Read: Irregular Periods: Unveiling the Underlying Causes
Vulvar Cancer
Vulvar cancer, a rare form of cancer affecting the outer surface of the female genitalia such as the labia and clitoris, constitutes less than 5% of all gynecologic cancers. In the United States, approximately 6,500 new cases of vulvar cancer are diagnosed annually.
Risk Factors Factors contributing to vulvar cancer include HPV infection, smoking, and chronic vulvar inflammation like lichen sclerosus. Notably, age is a significant risk factor, with most cases occurring in women aged 50 and above.
Symptoms and Signs Typical symptoms of vulvar cancer encompass persistent itching, pain, and noticeable skin changes such as Intractable dryness. Early detection plays a pivotal role in enhancing treatment outcomes.
Diagnosis and Staging Diagnosis involves a series of procedures including physical examination, biopsy, and imaging tests to ascertain the disease’s extent. Staging is determined by factors like tumor size, location, and spread to nearby lymph nodes or organs.
Treatment Options Treatment strategies for vulvar cancer hinge on the disease’s stage and severity. Common approaches include:
- Surgery: Typically entails the removal of cancerous tissue along with a margin of healthy tissue.
- Radiation Therapy: Administered post-surgery to diminish the risk of recurrence.
- Chemotherapy: Considered for advanced or recurrent cases. In certain instances, a combination of these therapies may be prescribed. Targeted therapy and immunotherapy are also potential components of treatment plans.
Prevention and Early Detection
Prevention and early detection play vital roles in managing gynecological cancers. Here are some key prevention measures and early detection strategies:
Prevention:
- HPV vaccination: Protects against the strains of HPV responsible for most cervical, vaginal, and vulvar cancers, and anal throat cancers.
- Regular screening: Aids in identifying precancerous conditions early, enabling prompt intervention.
- Practicing safe sex: Condom use and limiting sexual partners can reduce the risk of HPV transmission.
- Avoiding tobacco products: Smoking increases the likelihood of developing cervical and vulvar cancers.
Early Detection:
Early detection significantly improves outcomes for gynecological cancers. While screening tests like the Pap test and HPV test are available for cervical cancer, there aren’t reliable screening methods for other types. Hence, it’s crucial to be aware of warning signs and discuss individual risk factors with healthcare providers for potential interventions.
In conclusion, gynecological cancers pose significant health risks to women worldwide, but understanding their types, risk factors, symptoms, and available treatments is crucial for prevention and early detection. By prioritizing gynecological health, staying informed, and engaging in preventive measures such as vaccination, regular screenings, safe sexual practices, and avoiding tobacco products, individuals can take proactive steps toward reducing their risk and contributing to the global fight against gynecological cancers. Empowered with knowledge and awareness, we can strive for better outcomes, improved treatments, and ultimately, the eradication of these diseases as public health concerns.
For personalized guidance and consultation, book your appointment with Dr. S. Sharma at Sanjivini Super Speciality Hospital, Lucknow.
FAQS
- What are the risk factors for cervical cancer?
Risk factors include HPV infection, early sexual activity, multiple sexual partners, smoking, and a history of sexually transmitted infections.
- What are the primary screening methods for cervical cancer?
The Pap smear and HPV test are the primary screening methods.
- What are the common symptoms of ovarian cancer?
Symptoms may include bloating, pelvic discomfort, changes in bowel habits, and unusual fatigue.
- How is uterine (endometrial) cancer diagnosed?
Diagnosis typically involves an endometrial biopsy and imaging techniques such as CT scans or MRIs.