Medically Reviewed by: Dr. Sonali Sharma MD- GYNAE & OBS
Welcome to our blog on the HPV vaccine and its role in shielding against cervical cancer. In India, cervical cancer is a significant health concern for women, and understanding how to protect against it is crucial. Human Papillomavirus (HPV) is a common virus that can lead to cervical cancer, but vaccination offers a powerful defense. In this blog, we’ll explore what HPV is, why cervical cancer is a threat, and how the HPV vaccine can help safeguard your health. Let’s dive in and learn more about this important topic together.
Understanding HPV
Human Papillomavirus (HPV) is responsible for the majority of cervical cancer. Transmitted through sexual contact, persistent high-risk strains elevate cervical cancer risk. About 99.7% of cervical cancer cases involve HPV DNA, mainly HPV16 and HPV18. Cervical cancer ranks as the fourth most prevalent cancer in women globally, with around 604,000 new cases yearly.
HIV-positive women face a sixfold increased risk compared to the general population. Factors affecting cancer progression include HPV-type oncogenicity, immune status, other STIs, multiple childbirth early pregnancy, prolonged usage of hormonal contraceptives, and smoking. Prevention includes HPV vaccination, regular pre-cancer screening and treatment, smoking cessation, and barrier methods of contraception.
Also Read: Understanding the Different Types of Gynecological Cancers
Cervical Cancer: The Threat
Overview of Cervical Cancer
Cervical cancer is primarily caused by infections with high-risk types of human papillomavirus (HPV). Notably, HPV16 and HPV18 contribute to around 70% of cervical cancers globally. Other risk factors include smoking, weakened immunity, STIs, and prolonged sexual activity.
Impact on Women’s Health and Well-Being:
Cervical cancer poses a significant threat to women’s health. Timely detection and proper management greatly enhance survival rates. Routine screening, including Pap tests and HPV tests, can identify precancerous lesions, enabling swift intervention. Moreover, vaccination against specific high-risk HPV types offers preventive measures against cervical cancer.
HPV Vaccine: The Solution
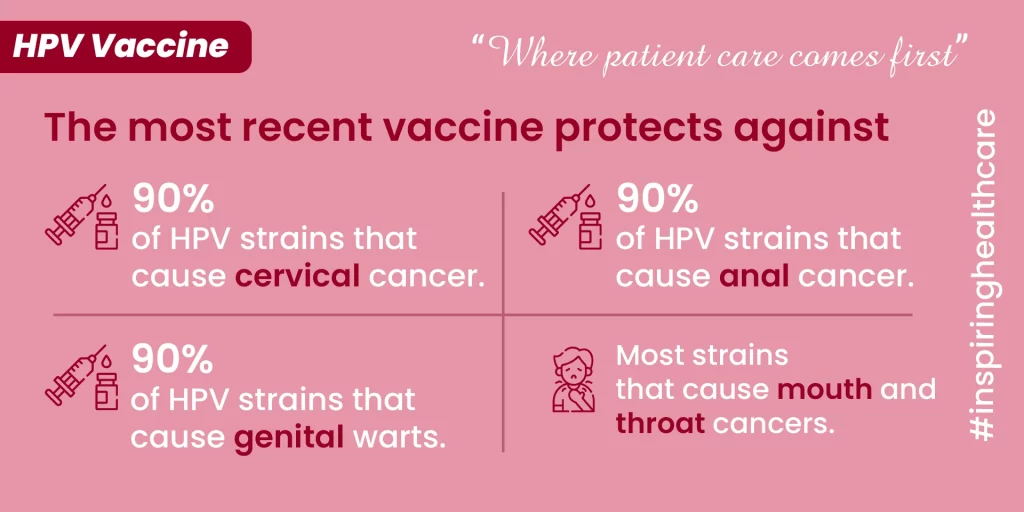
HPV vaccines play a critical role in safeguarding against infections caused by human papillomaviruses (HPV), which are associated with various cancers, notably cervical cancer.
How the Vaccine Works
HPV vaccines operate by stimulating the immune system to produce antibodies capable of identifying and neutralizing the virus upon exposure. These vaccines utilize virus-like particles (VLPs) that mimic the natural virus but are not infectious. By eliciting an immune response against these VLPs, the body can effectively combat HPV infections and decrease the risk of associated cancers.
- Gardasil 9: This vaccine prevents infection with four HPV types, including those causing genital warts and high-risk types like HPV16 and HPV18. Studies have shown its efficacy in preventing persistent infections and diseases linked to specific HPV types.
Effectiveness: Research has indicated the high efficacy of HPV vaccines in preventing persistent infections, cervical intraepithelial neoplasia (CIN), and adenocarcinoma in situ (AIS). Furthermore, these vaccines have demonstrated effectiveness against genital warts and anal intraepithelial neoplasia grade 2 or 3 (AIN 2/3).
Also Read: The Role of Proper Hygiene in Preventing UTIs (Urinary Tract Infections)
Who Should Receive the Vaccine
The Centers for Disease Control and Prevention (CDC) recommends HPV vaccination for children and adults aged 9 through 26 years. While vaccination is typically advised at age 11 or 12, it can commence as early as age 9. Additionally, adults both males and females aged 27 through 45 years can benefit from vaccination if not adequately vaccinated earlier.
Debunking Myths and Addressing Concerns
Common Misconceptions about the HPV Vaccine
Misconceptions about the HPV vaccine have stirred worries regarding its safety and effectiveness. Despite solid scientific backing supporting the vaccine’s safety and efficacy, there’s been a surge in parental concerns, largely due to misinformation and myths. Some false beliefs, like the vaccine causing infertility or autoimmune diseases, have been debunked by research.
Safety and Side Effects of the Vaccine
Scientific research confirms the safety of HPV vaccines, with benefits outweighing potential risks.
Addressing Concerns Regarding Vaccine Efficacy and Necessity
Studies demonstrate the high effectiveness of HPV vaccines in preventing HPV infections and related cancers. The quadrivalent HPV vaccine has significantly reduced HPV infections in female teens and young women since its launch in 2006. Despite this, concerns about vaccine necessity persist among parents, leading to hesitancy in vaccinating their children. Healthcare providers and public health leaders must tackle these concerns through education and communication to ensure broad vaccination coverage and reduce the burden of HPV-related diseases.
Importance of Vaccination
Public Health Impact of HPV Vaccination in India
HPV vaccination significantly reduces HPV infections and related cancers, making it pivotal for public health. Combined with cervical screening, it provides maximum protection against cervical cancer. Moreover, HPV vaccination lowers the risk of other HPV-caused cancers like oropharyngeal, vulvar, vaginal and anal cancers. Widespread vaccination could slash cervical cancer cases globally by up to 90%, also lessening the need for follow-up care, biopsies, and invasive procedures linked with abnormal cervical screening.
Healthcare Providers’ Role in Encouraging Vaccination
Healthcare providers are key influencers in advocating HPV vaccination. By educating patients about its safety and effectiveness, they dispel misconceptions and encourage higher vaccination rates. It’s crucial that providers actively recommend the vaccine to eligible individuals, stressing its role in preventing HPV-related cancers and boosting public health.
Ensuring Vaccine Access and Breaking Barriers
Overcoming barriers to vaccination requires ensuring widespread access to HPV vaccines. Efforts should focus on increasing awareness about vaccination benefits, addressing safety concerns, and expanding access to healthcare services offering the vaccine. Public health campaigns, school-based vaccination programs, and community outreach initiatives can enhance vaccination rates and bridge gaps in preventive healthcare access.
These measures are vital steps toward safeguarding public health and reducing the burden of HPV-related diseases in India.
In conclusion, HPV vaccination stands as a powerful shield against cervical cancer and other HPV-related diseases. By significantly reducing the incidence of HPV infections and related cancers, it plays a crucial role in safeguarding public health. We urge everyone to take action by getting vaccinated and spreading awareness about the importance of HPV vaccination.
Remember, your healthcare provider is your ally in this journey towards prevention. If you have any questions or concerns about HPV vaccination, don’t hesitate to reach out and consult with a healthcare professional. For personalized guidance and expert advice, book your consultation with Dr. S. Sharma at Sanjivini Super Speciality Hospital, Lucknow.
Let’s take proactive steps to protect ourselves and our loved ones from the threat of cervical cancer. Together, we can make a difference in promoting healthier communities and a brighter future for all.
FAQS
- What is HPV vaccination?
- HPV vaccination is a preventive measure designed to protect against certain strains of the human papillomavirus (HPV) that can lead to cervical cancer and genital diseases.
- Who should get the HPV vaccine?
- The HPV vaccine is recommended for both males and females, typically starting at ages 9 to 12, and up to age 26 for those who haven’t been vaccinated before.
- Is the HPV vaccine safe?
- Yes, extensive research and monitoring have shown that the HPV vaccine is safe and effective in preventing HPV infections and related cancers.
- How many doses of the HPV vaccine are required?
- Most individuals need two doses of the HPV vaccine if they start the series before age 15. If they begin vaccination at age 15 or older, three doses are recommended.
- Can the HPV vaccine prevent all types of HPV-related cancers?
- While the HPV vaccine primarily targets cervical cancer, it also protects against other HPV-related cancers, such as anal, vulvar, vaginal, and oropharyngeal cancers.

